What is Ulcerative Colitis?
Ulcerative colitis (UC) is a chronic inflammatory bowel disease in which inflammation and ulcers occur in your large intestine (colon) and rectum. It is most commonly thought to be caused from an overactive immune response. Normally, a viral or bacterial threat in your colon would trigger your immune system to cause temporary inflammation and send white blood cells to the area to combat an infection. The inflammation would go down once the body had successfully fought off the virus or bacteria present.
In UC, the immune system continues to cause inflammation and send white blood cells to the colon, which causes chronic inflammation and the forming of ulcers. The ulcers can produce pus and mucus, causing cramping, pain, and a feeling of needing to have frequent bowel movements to feel better. Symptoms generally flare, leaving the person in periods of a remission where they don’t experience as much pain or symptoms.
Signs and Symptoms of Ulcerative Colitis:
- Diarrhea, which can have blood or pus in it
- Urgent need for bowel movements
- Inability to empty bowels, despite urgent sensations
- Pain and cramping in your stomach
- Pain or bleeding in the rectum
- Weight loss
- Fatigue
- Fever
- Failure to grow in younger children
The symptoms are mild to moderate for most who suffer, but some experience severe symptoms, pain, and complications. Even moderate symptoms can interfere with the ability to normally function and perform work duties.
How is Ulcerative Colitis Diagnosed?
The diagnosis of chronic immune diseases is tricky. The most important thing is to be educated and prepared before you begin the journey to get a diagnosis. Your medical history, physical exam, and a thorough written documentation of symptoms with severity and frequency, will be extremely important in the process.
Doctors may perform the following tests to determine what the cause of your pain and symptoms is:
- Blood tests– a blood test can check for anemia, which could indicate bleeding in your colon or rectum, and signs of infection
- Stool samples– this can help a doctor determine is there is a parasite, virus, or bacteria causing your symptoms
- Colonoscopy– this procedure allows a doctor to thoroughly examine your colon and rectum, looking for polyps, ulcers, and take tissues samples, which are often necessary for official diagnosis
- X-Rays or CT Scans– a doctor may order an x-ray or CT scan to check for perforations, inflammation, blockages, or to see if there are any other physical complications that show up
C&P Exam Prep and VA Ulcerative Colitis Ratings
- Begin logging your symptoms. Seeing the dates, frequency and types of symptoms you are suffering from, as well as their impact on your life, is extremely important for a medical diagnosis to help you obtain service connection for ulcerative colitis.
- As always, for disability benefits, you’ll need:
- In-service event, illness, injury
- Current diagnosis from a medical professional
- Medical Nexus (link) between the in-service event, illness or injury and your current symptoms and diagnosis
- Lay statements from friends, family, or colleagues, can also be very beneficial. This helps a medical professional and the VA see how your pain and symptoms are affecting your ability to function normally in life, at home and at work.
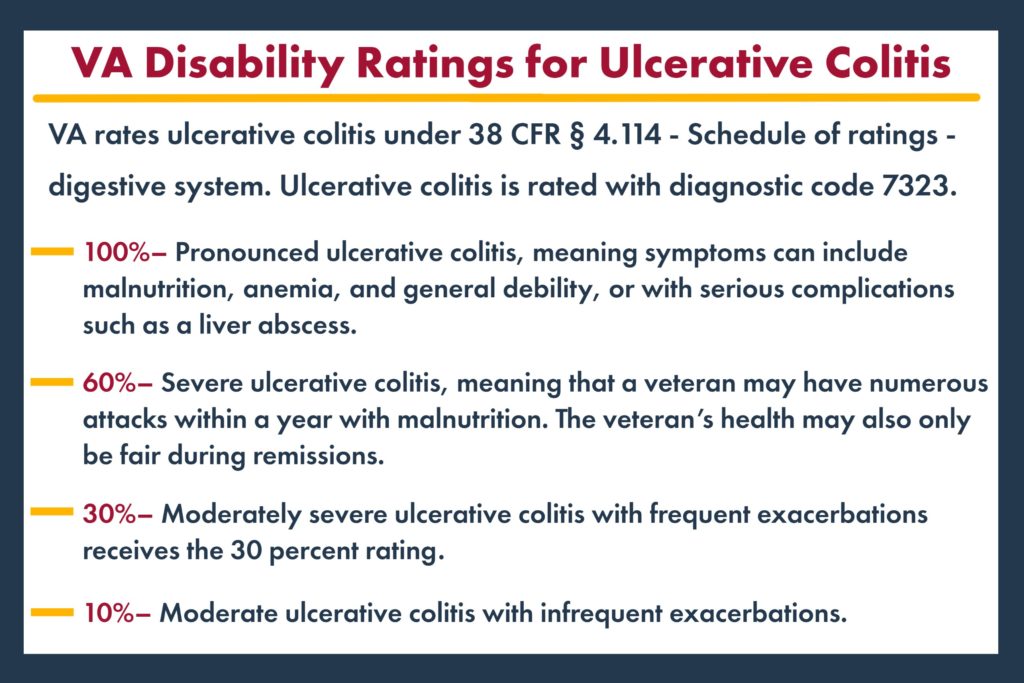
The VA rates ulcerative colitis under 38 CFR § 4.114 – digestive system, diagnostic code 7323.
Chart from CCK-Law website.
Ulcerative Colitis and Secondary Service Connections
There are many other conditions that ulcerative colitis can be linked to. Some of the most common are Post Traumatic Stress Disorder (PTSD), endometriosis, and other gastrointestinal and irritable bowel conditions or issues.
Treatment Options
Treatment for ulcerative colitis is often a combination of medication, diet and lifestyle changes, and less commonly, surgery to remove negatively affected areas in the colon.
- Medication – Anti-inflammatory drugs can be helpful for some people suffering from UC, as they allow the tissue in the colon and rectum to heal. Immune system suppressors are another common treatment for UC. These can reduce the frequency of UC flare ups and decrease the white blood cells being sent to the colon in immune response.
- Diet and Lifestyle – Many UC sufferers connect certain foods with triggering or exacerbating their symptoms and flare ups. The most common “trigger” foods are: spicy foods, caffeine and alcohol, foods high in fiber, anything with nuts and seeds, dairy products, greasy or fried food, and raw cruciferous vegetables. Maintaining a food diary can be helpful in determining which foods aggravate symptoms. Working with a medical professional or a nutritionist who specializes in colitis diet changes can be a good option.
- Surgery – 25-33% of people suffering find that medications and diet/lifestyle changes aren’t having a positive enough effect on systems or frequency, OR experience complications from the medications. In more severe cases, surgery may be recommended. Surgery generally involves removal of some, or all, of the colon.
Additional Resources
Connect with Us
Our team can help you navigate the complexities of the VA rating and benefit process. Many veterans are underrated and not receiving the maximum benefits and compensation that they have earned and deserve. Use the button below to connect now for a free consultation to determine if you are receiving your maximum!
Click Here for Info on Your Free Consultation
- Need some convincing? Read our Better Business Bureau and Google reviews here!